Growing Pains or Early Joint Disease? Orthopaedic Red Flags in Children
By Dr. Aman Dua, Best Orthopedic Surgeon in Delhi
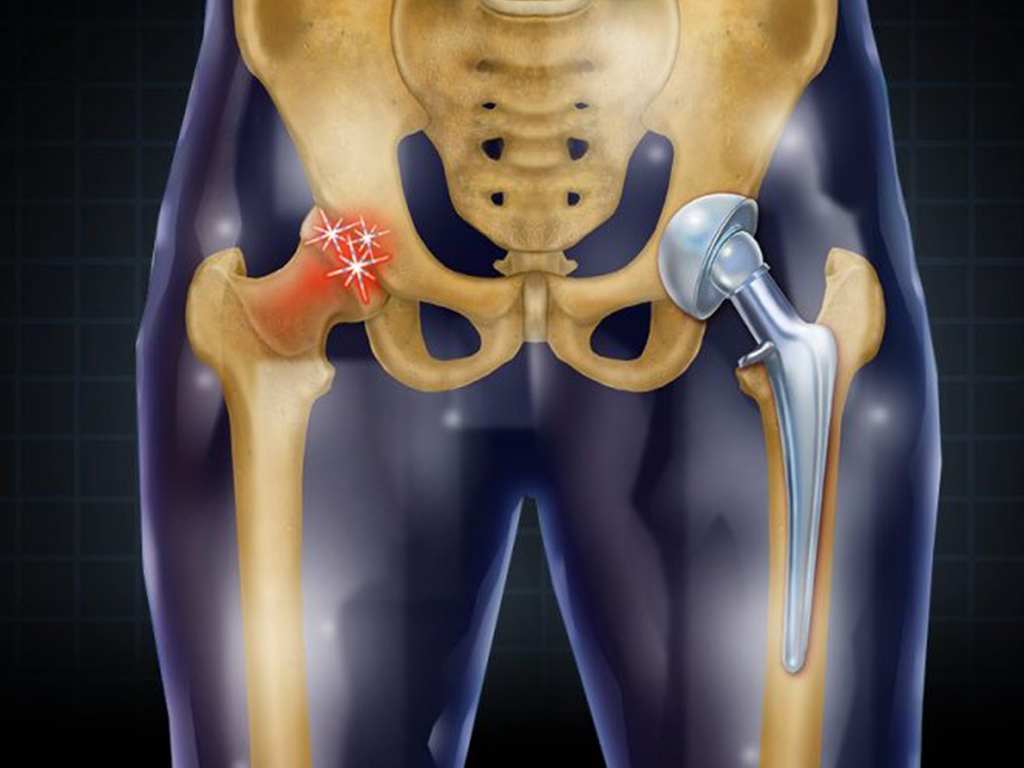
When a Child’s Joint Pain Should Not Be Ignored
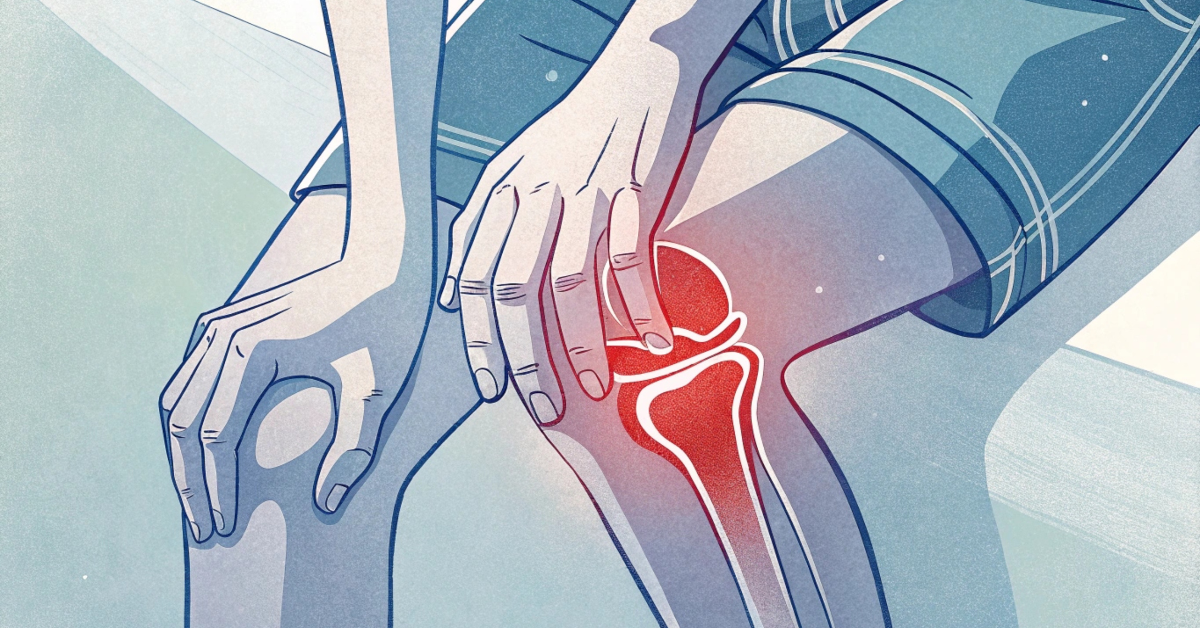
Persistent limping, knee pain, or difficulty walking may signal early joint, hip or growth plate problems rather than simple growing pains.
Timely orthopaedic evaluation can prevent permanent deformity and lifelong joint damage.